Dental Bone Loss Causes and Treatments
Have you ever run your tongue along your gumline and noticed your teeth seem longer than before? Or perhaps you’ve been told you have “receding gums” during a dental checkup? You might be experiencing dental bone loss – a condition that affects millions but often goes unnoticed until it’s advanced.
I remember my aunt complaining about her “teeth getting longer” as she aged. Little did she know, it wasn’t her teeth growing – it was her jawbone shrinking away. This silent condition can have serious consequences for your oral health and overall wellbeing.
In this comprehensive guide, I’ll walk you through everything you need to know about dental bone loss – from what causes it to how it can be treated and even reversed in some cases. Whether you’re concerned about your own oral health or researching for a loved one, this article will equip you with the knowledge to make informed decisions.
What Is Dental Bone Loss?
Dental bone loss (also called alveolar bone loss) occurs when the bone that surrounds and supports your teeth begins to deteriorate. This bone, known as the alveolar bone, is vital for holding your teeth firmly in place.
When it starts to diminish, you might notice:
- Teeth appearing longer
- Increased tooth sensitivity
- Loose teeth
- Changes in your bite
- Difficulty chewing
The scary thing about dental bone loss is that it often progresses without pain, making it easy to miss until significant damage has occurred.
The Main Causes of Dental Bone Loss
Periodontal Disease
The number one culprit behind dental bone loss is periodontal (gum) disease. This bacterial infection starts with inflammation of the gums (gingivitis) and, if left untreated, progresses to periodontitis – where the infection damages the bone supporting your teeth.
The bacteria release toxins that trigger an inflammatory response, causing the body to essentially turn on itself. Your immune system, trying to fight the infection, inadvertently breaks down the bone tissue.
Tooth Loss
Here’s something that surprised me when I first learned about it: “Use it or lose it” applies to your jawbone too! When a tooth is extracted or falls out, the bone that once supported it no longer receives the stimulation it needs from chewing and biting forces.
Without this stimulation, the bone begins to resorb (break down) – a process that can begin as soon as 6 months after tooth loss and continue throughout life. This is why people who have been missing teeth for years often develop a “sunken” appearance to their face.
Other Contributing Factors
Several other conditions can contribute to dental bone loss:
- Osteoporosis: This systemic bone disease can affect the jaw just like other bones in the body.
- Poor oral hygiene: Neglecting your dental care allows bacteria to flourish.
- Smoking: Reduces blood flow to the gums and weakens the immune system.
- Hormonal changes: Particularly in women during pregnancy or menopause.
- Misaligned teeth: Creates areas that are difficult to clean, leading to bacterial buildup.
- Certain medications: Some drugs can contribute to dry mouth or affect bone metabolism.
- Genetics: Some people are simply more susceptible to periodontal disease.
How to Stop Dental Bone Loss
The good news is that dental bone loss can absolutely be stopped with proper intervention. Here’s how:
- Treat the Underlying Cause
If periodontal disease is the culprit, addressing it is the first step:
- Professional dental cleaning: Removes plaque and tartar buildup.
- Scaling and root planing: A deep cleaning procedure that removes bacteria from below the gumline.
- Antibiotics: May be prescribed to control bacterial infection.
- Periodontal surgery: For advanced cases, surgical intervention may be necessary to clean areas inaccessible by other means.
- Improve Your Oral Hygiene Routine
Never underestimate the power of a good oral hygiene regimen:
- Brush twice daily with a soft-bristled toothbrush
- Floss daily to remove plaque between teeth
- Use an antimicrobial mouthwash
- Consider an electric toothbrush, which can be more effective at removing plaque
- Regular Dental Check-ups
Early detection is crucial. Regular dental visits allow your dentist to:
- Monitor your bone levels through X-rays
- Identify early signs of gum disease
- Provide professional cleanings to remove tartar buildup
- Offer personalized advice for your specific situation
- Lifestyle Changes
Several lifestyle modifications can help protect your dental bone health:
- Quit smoking: Smoking significantly increases your risk of bone loss.
- Maintain a balanced diet: Ensure adequate calcium and vitamin D intake.
- Control blood sugar: If you have diabetes, keeping it under control can help prevent bone loss.
- Manage stress: Chronic stress can weaken your immune system and exacerbate inflammation.
FAQs
What Causes Bone Loss Around Dental Implants?
Bone loss around dental implants (peri-implant bone loss) can occur for several reasons:
- Bacterial infection: Just like natural teeth, implants can harbor bacteria that cause inflammation and bone destruction.
- Excessive mechanical forces: If your bite isn’t properly balanced, excessive pressure on the implant can lead to bone loss.
- Foreign body reaction: Though rare, some people may have a reaction to the implant material.
- Poor surgical technique: The way the implant is placed can affect long-term bone stability.
- Systemic health conditions: Certain medical conditions like uncontrolled diabetes can compromise healing and bone maintenance.
Regular check-ups with your dentist are crucial for monitoring implant health and catching any issues early.
This is perhaps the most common question I hear about this condition. The answer is both yes and no – it depends on several factors.
Complete reversal of natural bone loss is not typically possible. Once bone is lost, regenerating it fully to its original state is challenging. However, there are treatments that can halt the progression and even rebuild some of the lost bone.
The extent to which bone can be regenerated depends on:
- The severity of the bone loss
- The location in the mouth
- Your overall health
- How quickly treatment is sought
Modern dentistry offers several approaches to rebuilding lost bone, which I’ll discuss in detail below.
Dental Bone Grafting: Rebuilding What’s Lost
When significant bone loss has already occurred, dental bone grafting offers a way to rebuild the lost structure. This procedure involves placing grafting material into the area of bone loss to stimulate new bone growth.
Types of Bone Grafts
There are several types of bone grafts used in dentistry:
| Graft Type | Source | Benefits | Considerations |
|---|---|---|---|
| Autografts | Your own body | Highest success rate, no rejection risk | Requires second surgical site |
| Allografts | Human donors | No second surgical site needed | Slight risk of disease transmission |
| Xenografts | Animal sources (typically cow) | Readily available | May take longer to integrate |
| Alloplasts | Synthetic materials | No biological source needed | May not integrate as well as natural bone |
The grafting procedure typically involves:
- Numbing the area with local anesthesia
- Creating a small incision in the gum tissue
- Placing the grafting material
- Securing the graft with a membrane
- Closing the gum tissue with sutures
Recovery usually takes several months as the graft integrates and new bone forms. During this time, you’ll need to:
- Follow a soft food diet initially
- Avoid putting pressure on the surgical site
- Take prescribed antibiotics to prevent infection
- Attend follow-up appointments to monitor healing

Do Dental Implants Prevent Bone Loss?
Yes! One of the most significant benefits of dental implants is their ability to prevent further bone loss. Unlike dentures or bridges, implants replace the entire tooth structure – including the root.
The titanium post of an implant functions similarly to a natural tooth root, transmitting chewing forces to the jawbone. This stimulation signals the body to maintain the bone, preventing the resorption that typically follows tooth loss.
Research has shown that dental implants can:
- Preserve existing bone
- Stimulate bone growth around the implant
- Maintain facial structure and appearance
- Provide a long-term solution for missing teeth
Do Dental Implants Cause Bone Loss?
While dental implants generally prevent bone loss, there are circumstances where implants themselves can contribute to bone loss:
Peri-implantitis
This is an inflammatory condition similar to periodontal disease but affects the tissues around an implant. It can lead to bone loss and potentially implant failure if not treated.
Signs of peri-implantitis include:
- Redness and swelling around the implant
- Bleeding when brushing
- Deepening pockets around the implant
- Exposure of implant threads
- Mobility of the implant
Improper Placement
If an implant is placed incorrectly or there’s excessive pressure on it, bone loss can occur. This emphasizes the importance of choosing an experienced implant dentist.
Smoking and Poor Oral Hygiene
Just as with natural teeth, smoking and inadequate oral hygiene increase the risk of complications with implants, including bone loss.
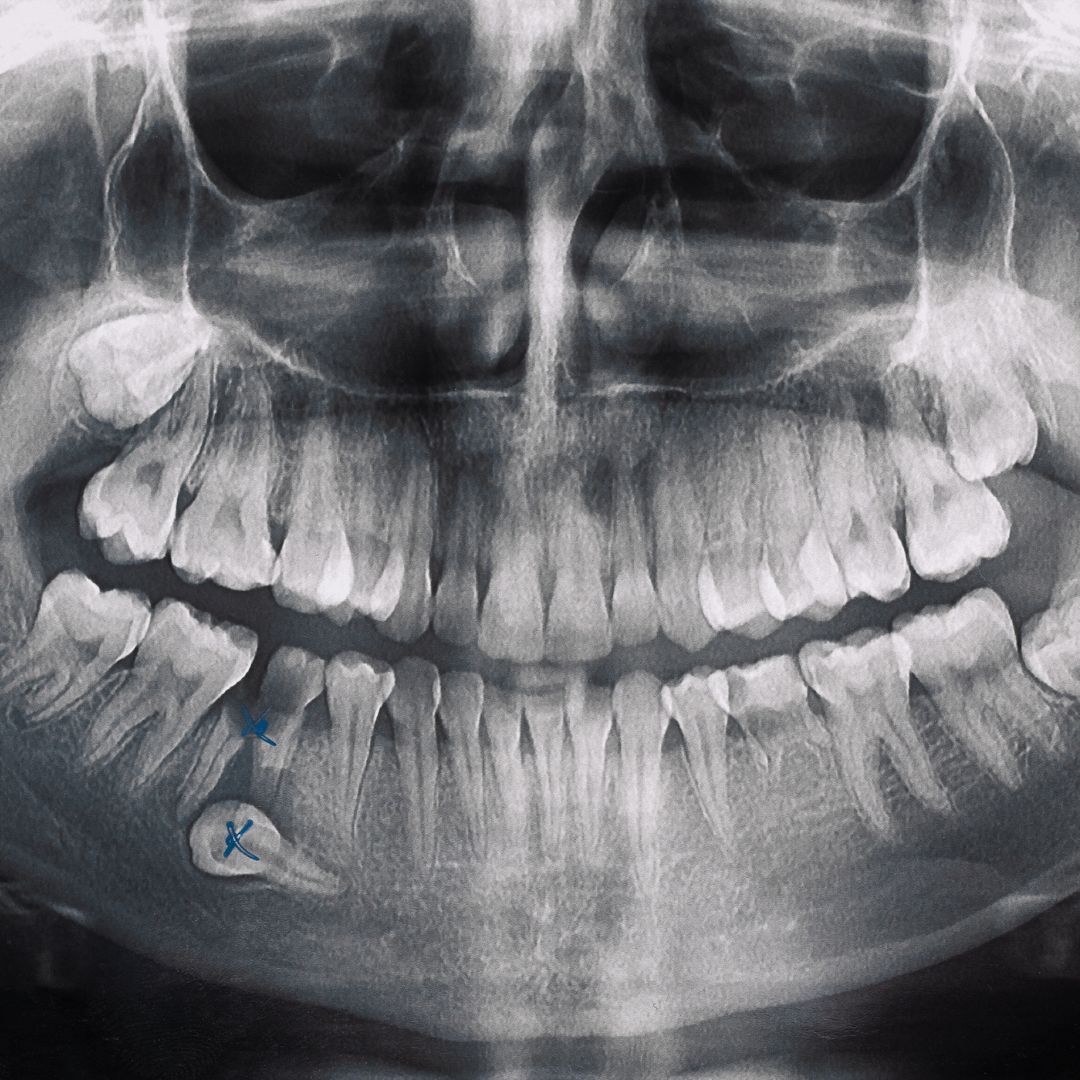
How to Read Dental X-rays for Bone Loss
Understanding your dental X-rays can help you be more engaged in your treatment. Here’s what to look for:
![Insert image of dental X-ray with annotations showing bone loss here]
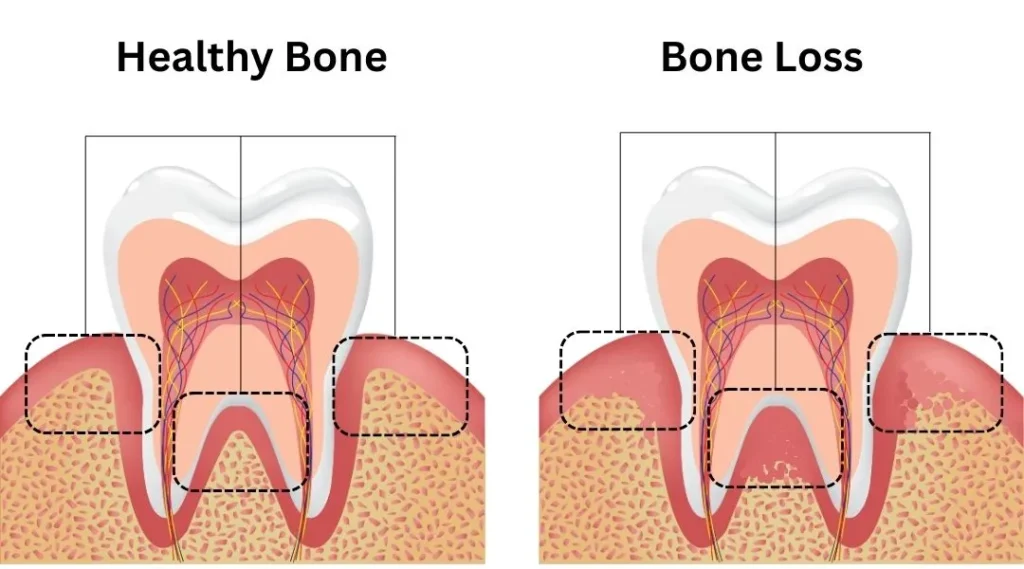
Healthy Bone vs. Bone Loss
In healthy teeth, the bone level should be about 1-2mm below where the enamel meets the root (the cementoenamel junction or CEJ). On X-rays:
- Healthy bone: Appears as a white line that follows the contour of the teeth roots, with the peak of bone between teeth forming a triangle shape.
- Bone loss: Shows as a darker area where the white line of bone has receded from the tooth.
Types of Bone Loss Patterns
X-rays can reveal different patterns of bone loss:
- Horizontal bone loss: The bone recedes evenly across multiple teeth (common in generalized periodontal disease).
- Vertical bone loss: Creates angular defects or “pockets” alongside individual teeth (often more severe).
- Furcation involvement: Bone loss between the roots of multi-rooted teeth.
Remember that X-rays are just one tool your dentist uses. They’ll combine this information with clinical examination findings to determine the full extent of bone loss.
Taking Control of Your Dental Bone Health
Dental bone loss may be common, but it doesn’t have to be inevitable. With proper care, early intervention, and modern treatment options, you can protect your jawbone and maintain a healthy, functional smile for life.
If you’re concerned about bone loss, don’t wait until symptoms become severe. Schedule an appointment with your dentist for a comprehensive evaluation, including X-rays to assess your bone levels.
Remember:
- Early detection is key
- Consistent oral hygiene helps prevent bone loss
- Regular dental visits allow for monitoring and intervention
- Even advanced bone loss can often be addressed with modern treatments
Your dental health is an integral part of your overall wellbeing – and it’s never too late to take steps to preserve it.
Have you dealt with dental bone loss? What treatments worked for you? Share your experience in the comments below!
References
- Jeffcoat MK, Reddy MS. Progression of probing attachment loss in adult periodontitis. J Periodontol. 1991;62(3):185-189. https://pubmed.ncbi.nlm.nih.gov/8122514/
- Bianchi ML, Bardella MT. Bone and celiac disease. Calcif Tissue Int. 2002;71(6):465-471. https://www.sciencedirect.com/science/article/abs/pii/S1297319X04000776
- Taguchi A, Tanimoto K, Suei Y, Wada T. Tooth loss and mandibular osteopenia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(1):127-132. https://pubmed.ncbi.nlm.nih.gov/11922263/
- Heaney RP, Recker RR, Saville PD. Menopausal changes in calcium balance performance. J Lab Clin Med. 1978;92(6):953-963. https://onlinelibrary.wiley.com/doi/abs/10.1002/jbmr.5650081307
This article is for informational purposes only and does not constitute medical advice. Always consult with a dental professional for diagnosis and treatment of dental conditions.
